The best NP job description clearly explains how nurse practitioners deliver patient centered care across primary and preventive care, acute care, and specialty settings while outlining real job responsibilities, scope of practice, and expectations. Employers who write a nurse practitioner job description that reflects daily clinical practice, autonomy in assessing patients, prescribing medications, interpreting diagnostic tests, and coordinating patient care attract certified nurse practitioners with the clinical expertise and professional knowledge needed to improve clinical outcomes.
Why NP Job Descriptions Matter More Than Ever
Nurse practitioner hiring has become more competitive as demand continues to rise across healthcare systems, private practices, hospitals, clinics, and emergency services.
Many nurse practitioners now serve as primary care providers, delivering primary and preventive care, managing chronic health conditions, responding to medical emergencies, and coordinating treatment plans across complex healthcare settings.
In this environment, the NP job description is no longer a formality. It is a critical signal of how an employer understands advanced practice nursing and supports clinical practice.
Many nurse practitioner job descriptions still rely on generic language that does not reflect modern nursing practice. They list degrees, certifications, and job requirements, but fail to describe how nurse practitioners actually treat patients, assess health conditions, order and interpret diagnostic tests, prescribe medications, or collaborate with other healthcare professionals such as physicians, physician assistants, and registered nurses.
Nurse practitioners invest years completing a bachelor’s degree, earning at least a master’s degree, gaining clinical experience, and obtaining national certification through professional organizations such as the American Nurses Credentialing Center. After this level of training, many nurse practitioners expect roles that fully use their clinical expertise in family medicine, acute care, mental health, pediatric health, or primary care settings.
That's why when job descriptions are vague or inaccurate, employers risk losing strong candidates who are looking for clarity around patient care responsibilities, autonomy, and collaboration within the healthcare team.
Clear, well-written NP job descriptions also support better outcomes beyond hiring. They help align expectations between employers and healthcare providers, reduce early turnover, and improve continuity of care for patients and families.
As healthcare systems continue to evolve, employers who treat the nurse practitioner job description as a strategic tool will be better positioned to attract experienced nurse practitioners, support effective patient care, and meet growing demands for high-quality medical care.
Common Problems With Traditional NP Job Descriptions
Despite the growing role of nurse practitioners across healthcare settings, many NP job descriptions have not evolved to reflect how advanced practice registered nurses actually work. These gaps create confusion for candidates and slow down nurse practitioner hiring by attracting the wrong applicants or discouraging qualified ones from applying at all.
They Focus on Credentials Instead of Clinical Practice
Many nurse practitioner job descriptions place heavy emphasis on degrees, certifications, and licensure while offering little insight into daily nursing practice. While requirements such as a bachelor’s degree, at least a master’s degree, national certification, and clinical experience are essential, they do not explain how the nurse practitioner will assess patients, examine patients, perform physical exams, or manage treatment plans. Candidates are left guessing how their professional knowledge will be applied in real patient care.
They Are Unclear About Scope of Practice
A common issue in NP job descriptions is vague language around scope. Many postings fail to explain whether the nurse practitioner will function as a primary care provider, manage acute care patients, support emergency rooms, or focus on preventive care and health promotion. Lack of clarity around responsibilities such as prescribing medications, ordering and interpreting diagnostic tests, managing pain, or performing minor surgical procedures creates uncertainty and limits applicant interest.
They Do Not Reflect the Healthcare Team
Nurse practitioners rarely work in isolation. They collaborate closely with physicians, physician assistants, registered nurses, and other healthcare professionals to coordinate patient care. When job descriptions do not explain how the nurse practitioner fits into the healthcare team or interacts with other health care providers, candidates struggle to understand expectations around collaboration, referrals, and shared decision-making.
They Miss the Real Patient Population
Many nurse practitioner jobs differ significantly based on setting and population. A family nurse practitioner in primary care may focus on disease prevention, health education, and promoting healthy lifestyle choices, while an acute care nurse practitioner may respond to medical emergencies and manage complex health conditions. Job descriptions that fail to specify patient populations, such as family health, pediatric health, mental health disorders, or acute care settings, make it difficult for many nurse practitioners to assess fit.
They Sound Generic Across All Settings
Too often, NP job descriptions are copied across hospitals, clinics, nursing homes, and private practices with minimal customization. This generic approach ignores differences in healthcare systems, patient needs, and clinical workflows. Nurse practitioners reviewing multiple postings quickly recognize when a job description does not reflect the reality of the role, which can reduce trust and engagement early in the hiring process.
What Nurse Practitioners Look For in Job Descriptions
Nurse practitioners read job descriptions very differently than many employers expect. They are not just scanning for job titles or requirements. They are looking for signals about how patient care is delivered, how the healthcare team functions, and whether the role supports sustainable clinical practice. Clear answers to these questions help qualified candidates decide whether to move forward.
Clear Scope of Practice and Autonomy
Nurse practitioners want to understand how they will practice on a daily basis. A strong NP job description explains whether the role functions as a primary care provider, supports acute care, or focuses on preventive care and health promotion. It should clearly outline responsibilities such as assessing patients, examining patients, prescribing medications, ordering and interpreting diagnostic tests, and referring patients when appropriate. Clarity around autonomy and decision-making helps advanced practice registered nurses evaluate whether the role aligns with their training and clinical expertise.
Defined Job Responsibilities and Clinical Focus
Many nurse practitioners look for detail around job responsibilities rather than broad statements. This includes the types of health conditions treated, involvement in treatment plans, participation in disease prevention, and expectations around patient education. Family nurse practitioners, acute care nurse practitioners, and mental health providers all have different clinical focuses. Job descriptions that reflect the real scope of patient care allow candidates to assess fit more accurately.
Transparency Around Patient Population and Setting
Nurse practitioners care deeply about who they will serve. Job descriptions should describe the patient population, such as family medicine, pediatric health, mental health disorders, or acute care patients. It should also clarify the healthcare setting, whether it is a clinic, hospital, emergency room, nursing home, or private practice. This context helps many nurse practitioners understand workload, acuity, and the pace of clinical practice.
Collaboration Within the Healthcare Team
NPs expect to work closely with physicians, physician assistants, registered nurses, and other health professionals. A strong nurse practitioner job description explains how care is coordinated, how referrals are handled, and how the healthcare team supports patient centered care. This transparency reassures candidates that collaboration and communication are valued parts of the role.
Growth, Support, and Professional Development
Many nurse practitioners are thinking long-term when evaluating a nurse practitioner job. They want to see signals that employers support continuing education, professional organizations, and clinical growth. Whether through mentorship, training, or exposure to different healthcare settings, job descriptions that acknowledge professional development help attract nurse practitioners who are committed to improving clinical outcomes and serving communities over time.
How to Write NP Job Descriptions That Work
Writing an effective NP job description requires moving beyond templates and focusing on how nurse practitioners actually practice medicine. The goal is to create a clear, accurate picture of the role so qualified candidates can quickly determine whether the position aligns with their training, experience, and approach to patient care.
Start With a Clear Role Summary
Begin with a concise overview that explains why the role exists and how it supports patient care. This section should clarify whether the position focuses on primary care, primary and preventive care, acute care, mental health, or a specialty area such as family medicine or pediatric health. A strong summary helps nurse practitioners immediately understand the purpose of the role within the healthcare system.
Describe Real Day-to-Day Clinical Responsibilities
Avoid vague language and focus on what the nurse practitioner will actually do. This includes assessing patients, performing physical exams, diagnosing health conditions, ordering and interpreting diagnostic tests, prescribing medications, managing pain, and coordinating treatment plans. If the role involves emergency services, minor surgical procedures, or managing medical emergencies, those responsibilities should be clearly stated. Specifics help candidates visualize the clinical practice and evaluate fit.
Clearly Define Scope of Practice
Scope of practice should never be implied. An effective nurse practitioner job description explains the level of autonomy, prescribing authority, and clinical decision-making expected in the role. It should also outline how the NP collaborates with physicians, physician assistants, registered nurses, and other healthcare professionals. Clear scope definitions support confidence, efficiency, and patient centered care.
Be Transparent About Schedule and Workload
Nurse practitioners want clarity around schedules before applying. Job descriptions should explain hours, shift structure, on-call expectations, and patient volume when possible. Transparency helps candidates assess workload, balance, and sustainability, especially in high-demand settings such as emergency rooms, acute care units, and busy primary care clinics.
Explain the Patient Population and Care Setting
Describe who the nurse practitioner will serve and where care is delivered. This may include families, children, older adults, or patients with chronic or acute health conditions. Clarifying whether the role is based in hospitals, clinics, nursing homes, private practices, or community settings helps many nurse practitioners understand pace, acuity, and expectations.
Outline Required Education and Certification Clearly
List required education and credentials in a clear, concise way. This may include a bachelor’s degree, at least a master’s degree, national certification, and clinical experience relevant to the role. Referencing certification through recognized professional organizations such as the American Nurses Credentialing Center helps candidates confirm eligibility without overwhelming them with unnecessary detail.
Use Clear, Professional Language
Write job descriptions in language that reflects respect for advanced practice nursing. Avoid jargon, inflated titles, or generic phrases that could apply to any role. Clear, direct language builds trust and helps nurse practitioners feel confident that the employer understands their profession and clinical expertise.
The Impact of Better NP Job Descriptions on Hiring Outcomes
Well-written NP job descriptions have a measurable impact on nurse practitioner hiring and overall workforce stability. When employers clearly define scope of practice, job responsibilities, and expectations, they attract candidates who are better aligned with the role and the needs of the healthcare team.
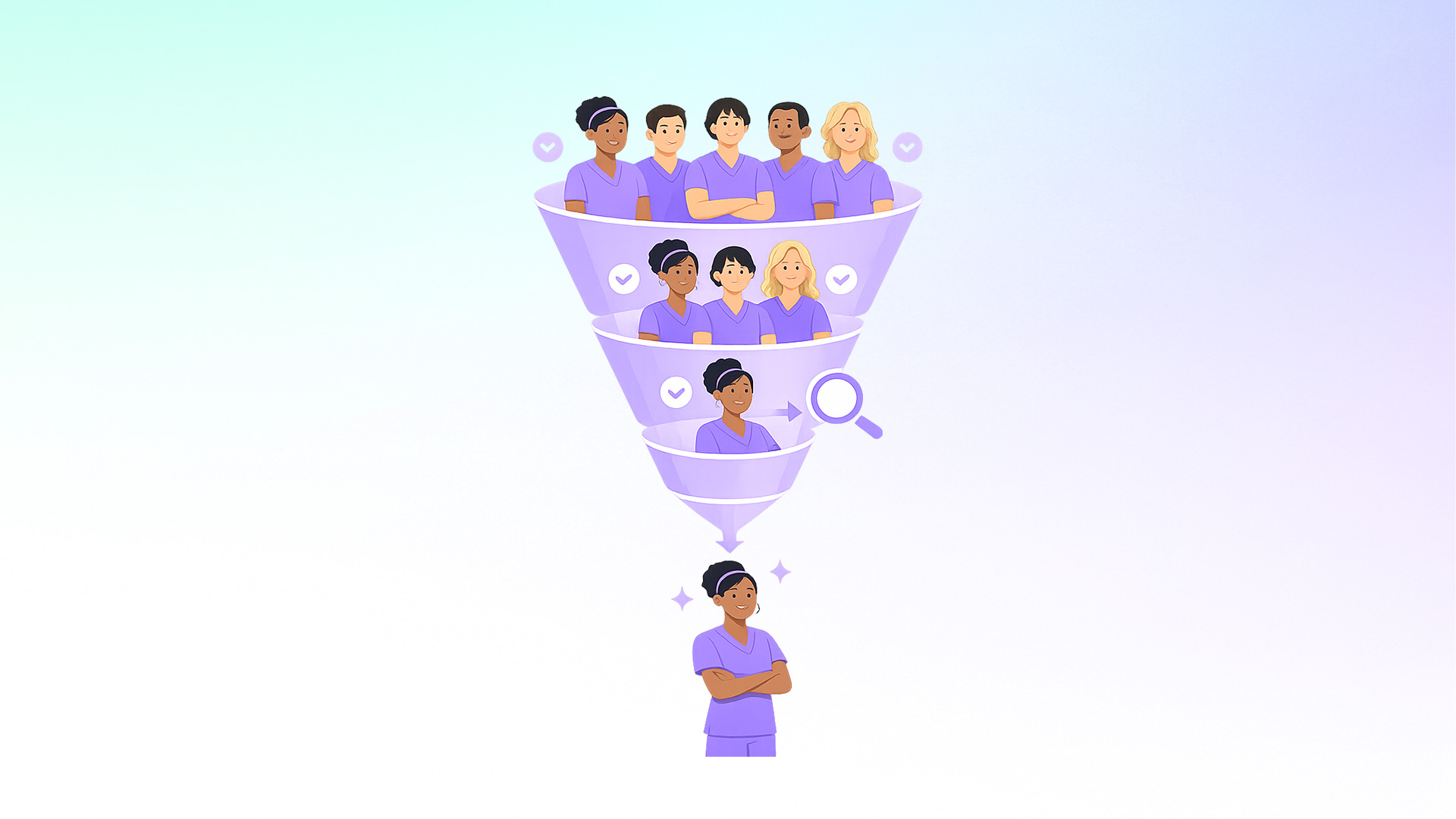
Clear nurse practitioner job descriptions lead to higher-quality applications. Candidates who understand the clinical focus, patient population, and care setting are more likely to apply when the role matches their clinical experience and professional interests. This reduces the number of unqualified applicants and allows hiring teams to focus on nurse practitioners who are ready to contribute from day one.
Improved clarity also shortens time-to-fill for nurse practitioner jobs. When expectations are transparent, candidates move more confidently through the hiring process. Interviews become more productive because discussions focus on clinical practice, collaboration, and patient care rather than clarifying basic role details. This efficiency supports faster hiring in high-demand areas such as primary care, acute care, and emergency services.
Better job descriptions also support retention and clinical outcomes. Nurse practitioners who join roles with a clear understanding of scope, workload, and team dynamics are more likely to stay engaged long term. This stability improves continuity of care, strengthens relationships with patients and families, and supports better clinical outcomes across healthcare settings.
For employers, investing time in accurate NP job descriptions reduces hiring friction, improves workforce planning, and supports sustainable care delivery. As job growth for nurse practitioners continues nationwide, clarity in job descriptions becomes a competitive advantage for healthcare systems seeking to attract and retain top clinical talent.
Common Mistakes to Avoid in NP Job Descriptions
Even well-intentioned employers often make avoidable mistakes when writing nurse practitioner job descriptions. These issues can discourage qualified candidates, slow hiring, and create misalignment that affects patient care after hire. Identifying and correcting these pitfalls helps ensure job descriptions support both recruitment and long-term success.
Using Physician or Generic Templates
One of the most common mistakes is copying job descriptions written for physicians or other healthcare professionals and lightly editing them for nurse practitioners. This approach fails to reflect advanced practice nursing and the unique role nurse practitioners play in patient care. NP job descriptions should clearly reflect nursing practice, scope of practice, and how nurse practitioners function as primary care providers or specialty clinicians within the healthcare team.
Overloading the Posting With Requirements
Listing every possible skill, certification, or experience can unintentionally narrow the candidate pool. While education such as a bachelor’s degree, at least a master’s degree, national certification, and relevant clinical experience should be included, excessive requirements can discourage strong candidates who are otherwise well qualified. Employers should focus on what is truly required for success in the role.
Hiding or Avoiding Key Details
Failing to include information about schedule, workload, patient population, or scope creates uncertainty for candidates. Nurse practitioners often skip postings that lack transparency around these factors. Omitting important details may increase application volume, but it often reduces quality and leads to longer hiring timelines.
Failing to Update Descriptions as Roles Evolve
Healthcare settings change, and so do nurse practitioner roles. Job descriptions that are not reviewed regularly may no longer reflect current responsibilities, patient populations, or care models. Outdated descriptions create misaligned expectations and can contribute to early turnover when reality does not match what was presented.
Writing Without Clinical Input
Job descriptions written solely by HR teams without input from clinical leaders or current nurse practitioners often miss critical nuances of the role. Including feedback from those involved in patient care helps ensure accuracy, clarity, and alignment with real-world practice.
Setting the Standard for NP Hiring
An outstanding nurse practitioner job description reflects how an employer understands nursing practice, values advanced practice registered nurses, and supports high-quality patient care.
As nurse practitioners increasingly serve as primary care providers, manage acute and chronic health conditions, respond to medical emergencies, and lead preventive care efforts, clarity in job descriptions directly shapes who applies, who accepts offers, and who stays.
When employers invest in writing accurate and detailed NP job descriptions, they establish clear expectations around scope of practice, clinical responsibilities, and collaboration within the healthcare team.
This allows nurse practitioners to assess alignment with their education, clinical experience, and professional goals before entering the hiring process. It also reduces misalignment that can lead to early turnover and disruptions in patient care.
Well-crafted job descriptions support better outcomes across healthcare systems. Nurse practitioners who understand their role are better positioned to assess patients, interpret diagnostic tests, prescribe medications, coordinate treatment plans, and deliver patient centered care across diverse healthcare settings.
Over time, this alignment strengthens clinical teams, improves retention, and supports more consistent, cost effective care for patients and families.
As demand for nurse practitioners continues to grow nationwide, employers who treat the nurse practitioner job description as a strategic hiring tool gain a clear advantage.
By reflecting real clinical practice, transparent expectations, and respect for advanced practice nursing, healthcare organizations can attract skilled nurse practitioners, support sustainable careers, and better serve the communities that depend on their care.
Frequently Asked Questions
1. What makes a strong nurse practitioner job description?
A strong nurse practitioner job description clearly explains scope of practice, daily clinical responsibilities, patient population, and how the NP collaborates with the healthcare team. Transparency helps qualified nurse practitioners assess fit before applying.
2. How detailed should job responsibilities be in an NP job description?
Job responsibilities should reflect real clinical practice. This includes assessing and examining patients, ordering and interpreting diagnostic tests, prescribing medications, managing treatment plans, and coordinating patient care across healthcare settings.
3. Should NP job descriptions include scope of practice details?
Yes. Scope of practice should be clearly defined, including autonomy, prescribing authority, and collaboration with physicians and other healthcare professionals. Clear scope supports confidence and efficiency in patient care.
4. Is it important to include patient population and setting?
Absolutely. Nurse practitioners want to know who they will serve and where care is delivered. Describing patient populations such as family health, pediatric health, mental health, or acute care helps candidates evaluate alignment.
5. Should compensation and schedule be included in NP job descriptions?
Including schedule expectations and compensation information improves transparency and reduces hiring delays. Nurse practitioners are more likely to apply when key details are shared upfront.
6. How often should nurse practitioner job descriptions be updated?
NP job descriptions should be reviewed regularly, especially when roles, patient populations, or care models change. Updated descriptions help prevent misaligned expectations and early turnover.
7. Who should be involved in writing NP job descriptions?
HR teams should collaborate with clinical leaders and practicing nurse practitioners. Input from those involved in patient care ensures accuracy and relevance.
8. Do better job descriptions improve NP retention?
Yes. Nurse practitioners who join roles with clear expectations around scope, workload, and collaboration are more likely to remain engaged and stay long term.
9. How do NP job descriptions affect time-to-fill?
Clear and accurate job descriptions attract more qualified candidates and reduce unnecessary interviews. This shortens time-to-fill and improves hiring efficiency.
10. Can a job description influence patient care outcomes?
Indirectly, yes. Clear job descriptions support better hiring decisions, stronger team alignment, and more consistent patient care, which improves outcomes for patients and families.





.webp)

.webp)

